Research Impact Report - Project 539
Improving shoulder hemiarthroplasty by using ceramics and preventing abnormal Biomechanics
Principal Investigator Ulrich Hansen
Stream PhD
Duration 24 Months
Cost £64,440

Lay summary
The shoulder is a ball and socket joint like the hip; arthritis of the shoulder is a common problem causing pain and loss of function. Shoulder replacement is a treatment option, but the outcome is poorer and medical research is less advanced than hip. In a significant number of patients it is not clear if they would be better in the medium to long term with a half new shoulder replacing the ball (hemiarthroplasty) or a full new shoulder replacing the ball and socket (total shoulder). This is an important question because total shoulder replacement is more invasive, has a higher risk of complications, a tendency to wear out if used heavily and are more expensive. The reason total shoulder replacements are more commonly used is that historically metal hemiarthroplasty has given inferior clinical outcomes, we plan to investigate if better outcomes are achieved using ceramic hemiarthroplasties.
The two main problems with total shoulder replacement are loosening of the artificial socket and failure of the muscles around the shoulder: this project aims to address these issues. Artificial sockets were inserted because traditional metal hemiarthroplasties rubbing on bone may have residual pain and stiffness, ceramic glides much better than metal potentially making these problems less likely, avoiding the need for a new socket and hence the problems with it wearing out. We want to work out if this is correct.
Turning to muscle failure, a major part of the problem is cutting muscles at the front to put in the new shoulder. For some years we have been investigating, in the laboratory, splitting (rather than cutting) the muscles at the back of the shoulder allowing access to insert a hemiarthroplasty. We want to examine further good and bad points of this approach before using it more extensively in patients.
The main symptoms of shoulder arthritis are pain and loss of function, with impact on the patients’ quality of life. There is also a societal burden in terms of inability to work, analgesic drugs, physiotherapy and in some cases packages of care.
Total shoulder replacement, particularly the reverse shoulder replacement, gives a good outcome in many patients. The main concerns relate to complication rates and longevity. Joint replacements wear out with time when this or other problems such as muscle failure occur, further surgery to remove the old replacement and insert a new one may be required, this is called a revision. Revision of a total shoulder replacement is technically demanding surgery, mainly related to the large amount of bone removed at the first operation.
If this project confirms that there are likely to be benefits from using ceramic hemiarthroplasty combined with minimally invasive bone sparing surgery there are a number of potential benefits to patients:
In the short term
- less traumatic surgery leading to reduced hospital stay, more rapid recovery times, fewer medical complications
In the long term
- Lower complications related to muscle failure
- Lower revision rates related to failure of the socket
- Related to the above increased replacement life span
- Technically easier revision surgery
Minimally invasive ceramic hemiarthroplasty is not a panacea and many patients will continue to be well treated by Reverse shoulder replacement. However, there is a demand for a solution for younger patients requiring shoulder replacement. If successful, our envisaged minimally invasive ceramic hemiarthroplasty procedure will offer these patients a better surgical option. If, in the long-term, a hemiarthroplasty fails, it may be revised to what is now a conventional total shoulder replacement.
Impact statement
Fundamental problem trying to address
Aims & Objectives
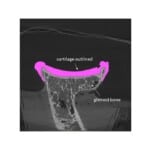
The main causes for high shoulder hemiarthroplasty revision rates are glenoid wear and rotator cuff dysfunction. The purpose of this project is to investigate if (1) using ceramic components and (2) an unconventional, muscle-sparing surgical approach can minimize glenoid wear and cuff dysfunction and thus reduce hemiarthroplasty revision rates.
- Conventional hemiarthroplasty uses metallic implants and high failure rates are reported (9-12%). In contrast, data from our clinic shows that ceramic bone-sparing hemiarthroplasties are associated with fewer revisions. Furthermore, our recent laboratory study found that ceramics cause 75% less damage to cartilage than metals. However, these clinical data are anecdotal and the laboratory findings preliminary. Therefore, ceramic hemiarthroplasty is promising but requires further evidence.
- During standard shoulder arthroplasty the rotator cuff is detached, but high rates of failure to heal are reported; a dysfunctional cuff causes abnormal joint biomechanics with instability and glenoid wear. We recently developed a unique surgical approach for shoulder replacement surgery that splits rather than cuts the cuff. Sparing the cuff should preserve normal joint biomechanics, avoid cuff dysfunction and failures. However, these potential gains need to be demonstrated.
We aim to demonstrate that the combination of ceramic hemiarthroplasty implanted using cuff-sparing surgery will reduce cartilage/bone erosion and cuff dysfunction. Importantly, this solution offers extraordinary minimal invasiveness as both bone and soft tissues are spared.
- To assess if ceramic humeral heads articulating against the native glenoid cause less glenoid wear than metallic humeral heads.
- To measure if joint loads representing normal shoulder biomechanics reduce glenoid wear relative to those with a dysfunctional cuff.
Deliverable: a recommendation if ceramic and/or a posterior surgical approach should be used in hemiarthroplasty.
Intellectual property
Ceramic implants are infrequently used for hemiarthroplasty but are commercially available (used regularly in our clinic). Hence, the implant is ‘ready’. Similarly, the surgical posterior approach is already used in arthroscopy of the shoulder and is ‘ready’. The purpose of the project is to increase the evidence base to motivate surgeons to use technology already available to the benefits of patients.
Clearly Mathys Ltd. which markets the ceramic implants would commercially exploit any findings supporting the use of ceramics. As such the company would support our and ORUK’s mission to deliver pain free function to patients.
If generation of IP emerges as a possibility the Enterprise Division (ED) at Imperial College London will support our project. ED will assist in the evaluation of the strength of the IP of the ideas stemming from this project, and in their commercialisation. If successful, ED will help with the IP protection and/or registration of the inventions. For this, ED liaises with patent attorneys for the preparation and submission of patent specification, providing also support at the different stages of the IPR prosecution. We have a successful collaboration with ED and they recently assisted us in the patent application for a novel ceramic humeral head.
Team members & other funders
- Ms Hazimah Mahmud (Bioengineer PhD student)
- Dr Dong Wang (Bioengineer, Lecturer U Exeter, and contracted consultant on the project)
- Mr Peter Reilly (Consultant Specialist Orthopaedic Shoulder surgeon)
- Dr Ulrich Hansen (Bioengineer, Senior Lecturer)
- Professor Andrew Amis (Bioengineer)
- Professor Daniele Dini (Tribologist, ie. Wear and tear of materials)
- Professor Roger Emery (Consultant specialist Orthopaedic Shoulder Surgeon)
Other Funders and collaborators:
- Mathys Medical (Orthopaedic implant manufacturer). Mathys has donated the implants for the study (42) as well as funding to cover purchase of cadaver specimens for study.
- Christian Heinrich’s (Mathys Medical), bioengineer. Provides industry perspective relevant to project
- Brunei’s Government provides a full scholarship for Ms Hazimah Mahmud’s PhD studies.
Publications
The following papers, both related to work package 2, are in draft format and likely to be submitted before end of 2021:
Mahmud H, Hansen U, Modenese L, Reilly P and Bull, A. Validating the glenohumeral joint reaction forces of the UK National Shoulder Model. Work to be submitted in short form to WCB and full study as a Technical note to J Biomech.
Mahmud H, Reilly P, Huang Y, Ackland D, Hansen U. Dysfunctional subscapularis increased the anterior-posterior glenohumeral joint reaction force during activities with large internal rotation. Ideally to be submitted to Journal of Shoulder and Elbow Surgery.
Links
https://pubmed.ncbi.nlm.nih.gov/31948834/
https://pubmed.ncbi.nlm.nih.gov/27745804/




Tell us your thoughts